Abstract
Abnormal adhesion of red and white blood cells (RBCs and WBCs) to the endothelium is a hallmark of sickle cell disease (SCD), and is not well elucidated. We have found that RBC adhesion profiles for different adhesion ligands on the (sub) endothelium, drawn at clinical baseline, associate with biomarkers of disease severity such as LDH and absolute reticulocyte counts. However, these adhesion profiles may change significantly for an individual over time. To better understand the implications of RBC adhesion relative to disease status, we monitored longitudinal RBC adhesion to laminin (LN), drawn during baseline clinic visits, in individual patients.
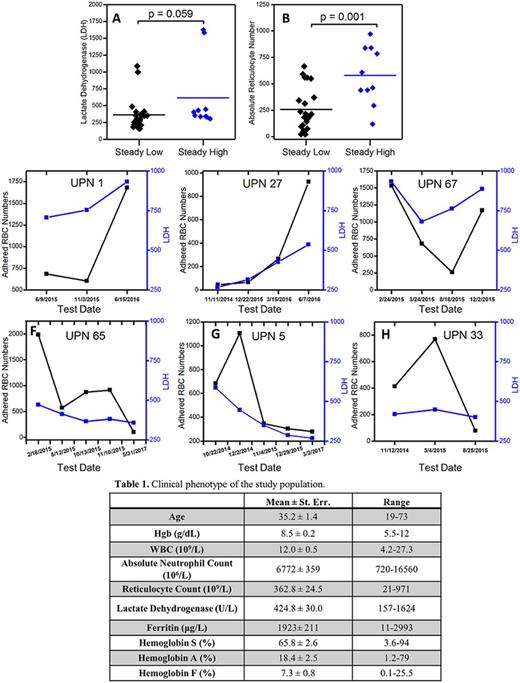
82 blood samples from 31 SCD patients (Table 1, 27 HbSS and 4 HbSS HPFH; 16 males and 15 females) were collected at the University Hospitals Seidman Cancer Center/CWRU in Cleveland, OH over the study period between October 2014 and July 2017. Adhesion experiments were performed by perfusing whole blood samples through LN-immobilized microchannels and quantifying the number of adherent RBCs in the channels following a rinse at physiological flow conditions. Consequently, patients were categorized into 3 groups based on their RBC adhesion numbers: stably low (<500), stably high (>500), and non-stable. Patients with non-stable adhesion had adhesion to LN that fluctuated between low and high.
We observed a higher mean LDH level in stably high patients compared to stably low patients (Fig. 1A, mean = 614.9±165.4 vs 361.4±48, p=0.059, one-way ANOVA). Compared with stably low adhesion, patients with stably high adhesion had significantly greater absolute reticulocyte counts (Fig. 1B, p=0.001, one-way ANOVA). Patients with non-stable RBC adhesion to LN show an association between individual LDH levels and adhesion at that time (Fig. 1C through 1H). However, an association was absent during several time periods, such as patient 67, 65, and 5 (Fig. 1E, 1F, and 1G).
Our data showed that SCD patients can broadly be separated into three groups based on the changes in their longitudinal RBC adhesion levels in LN-functionalized microchannels. Patient clinical data, particularly hemolytic biomarkers (LDH and absolute reticulocyte counts), correlated with the quantitative RBC adhesion numbers for patients with low and high adhesion. Furthermore, the general adhesion profile of patients with non-stable adhesion over time were generally consonant with their LDH levels, rather than pain profiles, which may suggest a hemolytic phenotype in those patients with increased RBC adhesion to LN, which may be pathophysiologically relevant. We are testing whether adhesion by RBCs to LN could be a useful surrogate for disease activity in therapeutic studies of anti-adhesive therapy.
Acknowledgments: This work was supported by grant R01HL133574 from the National Heart Lung and Blood Institute.
Figure 1. Longitudinal analysis of RBC adhesion to LN in SCD patients. Patients were categorized into three groups: stably low (<500), stably high (>500), and non-stable. Steady high patients had elevated LDH levels with a non-significant correlation (A) as well as significantly higher absolute reticulocyte counts. Change of RBC adhesion numbers to LN associated with patient LDH levels over time for (C) UPN 1, (D) UPN 27, (E) UPN 67, (F) UPN 65, (G) UPN 5, and (H) UPN 33. (UPN: Unique Patient Number)
Little: Hemex Health: Equity Ownership. Gurkan: Hemex Health: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal